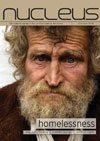
'There's a tramp asking to be seen today,' said the receptionist to the practice manager. She was not sure whether she should register this man, and if so, how. Was he 'immediate and necessary', or a 'temporary resident'? What should she put for his address? He said he was sleeping in the park.
The last time she let a 'tramp' into the surgery, patients complained to the manager about the smell in the waiting room, the doctor complained to the receptionist because he did not like alcoholics, and the practice nurse grumbled because she spent half an hour dressing his leg ulcers! The last straw was when he managed to leave without completing the paperwork. The manager said to fit him in if there was a free slot, and otherwise suggested he went to the hospital. As there were no spare appointments, the receptionist told him to go to accident and emergency (A&E), about a mile away. He limped away, looking sad.
A dark-skinned woman approached the window, saying, in broken English, 'I must see doctor'. The receptionist felt more confident here, because there was a policy. But she always found these people difficult, and she knew the doctors did not like them registering, because they took up so much time. She told the woman that she had to phone in the morning, to allow time to organise an interpreter. The woman did not understand, but sensing a rejection, spoke more forcefully, 'I must see doctor now!' The receptionist, conscious of the practice's zero tolerance policy towards aggression, thrust a multi-lingual leaflet into the woman's hands and closed the window. The woman could not read, and turned away in tears.
Do these scenarios resonate for you? Maybe your last encounter with a homeless person was during your A&E attachment, or in general practice. What about 'immigrants' who have limited or no English? Street homeless people and asylum seekers are among the more visible of the 'marginalised' or 'socially excluded' groups. But there are many others whose access to proper primary health care is jeopardised by the negative reaction of care providers.
Laws and loopholes
Under UK law, both the Race Relations Act 1976 (amended in 2000) and the Disability Discrimination Act 1995 (amended in 2006) govern how we provide healthcare. While the less well known but highly relevant 'right to health' (found in article 12 of the International Covenant on Economic, Social and Cultural Rights, ratified by the UK Government in 1968) [1] adds a moral, if not a legal, dimension.
Under the NHS, healthcare should be available to all UK citizens at the point of need, regardless of the nature of the health problem, race, religion, occupation, sexual orientation, or any other label. That term 'citizen' highlights one of the issues – there are rules determining entitlement to NHS care for non-citizens, whether European Community (EC) citizens, non-EC visitors, asylum seekers, and so-called 'failed' asylum seekers. [2]
But neither a street homeless person who is a UK citizen, nor an asylum seeker whose case is under consideration by the UK Border Agency (UKBA), fall into the category of those who are not entitled to NHS care. [2] So why do these scenarios seem so familiar?
Problems and prejudices
-
Consider the reasons why this hypothetical practice raised barriers to our homeless man:
- He had no fixed address
- He posed a threat to the waiting room environment and he might upset other patients
- He might increase the workload of the nurses
- He would probably not contribute to the practice's score in the Qualities and Outcomes Framework (a points-based system for payment to NHS GPs, largely focused on chronic disease management)
We could add that he was not the sort of patient they wanted to include on their list. And what about the woman with limited English? She failed to get help, despite the receptionist trying to follow procedures. The practice was not bending over backwards to help her, rather the reverse; there was a negative attitude at all levels:
- She could not understand the receptionist
- She could not read the literature, even in her own language
- She would need an interpreter, which would mean a longer consultation, and additional cost to the Primary Care Trust (PCT) or the practice itself
- She might have one or more 'difficult' conditions such as post-traumatic stress disorder (PTSD), TB, or HIV
Defining 'homeless people'
The group includes not only the visible 'street homeless' rough sleepers, but also people living in hostels, bed and breakfast accommodation, and people 'living with friends'. This entails sleeping on floors, and moving from flat to flat as their friends' patience or funds become exhausted. Homeless people have become homeless for a reason; often a relationship breakdown. This could be precipitated by a drug and alcohol addiction or other mental illness, commonly found in this group, both as a result of their homelessness and as a cause of it. [3]
Homeless people are far more likely to suffer from learning disability, making them more vulnerable and less able to seek help assertively. [4] Most of the failed asylum seekers discussed below will also be homeless in this latter sense, and indeed some will be sleeping rough. Homeless people do not usually have a telephone, and they find appointments difficult to keep. Some larger cities have services run by the PCT dedicated to the needs of 'socially excluded' people.
Asylum seekers and refugees
In addition to about 25,000 who now enter the UK each year claiming asylum, [5] there are an estimated 300,000 or more asylum seekers who have not yet been granted permission to stay. Their fate is in the hands of the UKBA, as well as the Asylum and Immigration Tribunal (the court that hears appeals and makes final decisions). After receiving permission to stay in the UK, asylum seekers are known as refugees. They become entitled to the same rights and benefits as UK citizens, and they are able to apply for citizenship themselves.
The mental health needs of refugees and asylum seekers are complex and serious. In particular, PTSD has to be identified or excluded. It is often accompanied by other psychiatric diagnoses, especially major depressive disorder. Good support from a mental health service is important, as there are very specific psychological treatments for this condition. [6] Torture, rape, and injuries such as gunshot wounds torture carry emotional and well as physical consequences.
People from sub-Saharan Africa (eg the Democratic Republic of Congo, Zimbabwe, Angola) are more likely to have HIV, for which specialist care is essential. HIV positive patients pose no special threat to primary care, provided that staff members know about the condition and precautions against blood-borne viruses.
Tuberculosis is a significant disease in vulnerable people. Although easily treated, a high index of suspicion is required, so that all potential cases are referred for screening at the local chest clinic. Asylum seekers are normally screened at the port of entry, and they may be followed up at their dispersal area by public health nurses. Other health issues of this group include poor nutrition and the physical consequences of torture, such as broken bones and gunshot wounds.
Limited English proficiency
Both asylum seekers and refugees are likely to have limited English proficiency (LEP), such that they need an interpreter in order to access healthcare. It is a requirement of all NHS providers to offer an interpreter when needed. Although this is a specific right for patients, the corresponding duty on NHS organisations is rather vague; I usually cite the Race Relations Acts and the Disability Discrimination Acts.
Organisations have different ways of meeting this obligation. Some, specialising in the care of asylum seekers and refugees, have a dedicated group of interpreters on call. Others will be able to call on a locally organised interpretation service, while for most it will be a commercial telephone interpreter service. These are of course always available, and while they may be 'second best' to a live and trained interpreter, they are far better than nothing, and would be quite appropriate for our scenario.
Practices in areas where refugees and asylum seekers live should ensure that their staff have some training in the needs of people with LEP. Clinical personnel need training in working with interpreters, as the consultation is quite different when a third person is involved. Many medical schools are beginning to include this skill in their consultation skills teaching programmes. If yours does not, why not make a request through your staff-student liaison process?
Failed asylum seekers
What about 'failed' asylum seekers? People who have exhausted the appeal process in their quest for asylum will have received a letter from the Home Office informing them that they are no longer entitled to housing support or even NHS care apart from in an emergency. However, the ruling of the High Court in April 2008 [2] overturned this unfortunate Department of Health directive. The 'Still Human Still Here' campaign [7] is seeking to change the law to extend support to such people.
For the present, general practitioners have considerable discretion in how they choose to apply the rules, and they are able to ensure this group is treated with dignity and compassion. There are both public health and humanitarian arguments for providing proper healthcare for destitute asylum seekers. Of course, the government is responsible for managing limited resources, but there is no evidence that the NHS is being exploited, rather the reverse. The financial cost of extending NHS care to this group is a tiny fraction of the NHS budget.
A Christian perspective
Given the legal framework I have outlined, you might ask, why should there be a particularly 'Christian' take on this? Despite the law, there is a huge variation in the way health professionals approach these vulnerable groups. Jesus is described as having 'compassion' [8] – a word with deeply visceral overtones, coming from the Greek word splanchizomai, 'to be moved as to one's inwards (splanchna), to be moved with compassion, to yearn with compassion'. [9] Hence in older versions of the Bible, 'bowels of mercy'. Can we share this degree of commitment?
Does our colour blind interpretation of the Bible fail to differentiate the Mediterranean Jesus, the black Simon of Cyrene, the black Ethiopian cabinet minister, and the many different races comprising the early church? [10,11] Have you ever turned a blind eye to discrimination? By doing nothing, you are complicit! Most medical schools have an organisation supporting refugees – perhaps you might join it. Christians can be 'salt' and 'light' beyond the comfort of the Christian Union or CMF group! Maybe there is a church-based 'drop-in' for destitute asylum seekers – your help might be much appreciated. Maybe your own church needs to be informed of the facts. [12] Many asylum seekers are Christians – some have been persecuted for their faith. Welcome them. Others come from an Islamic culture, but are very open to our friendship. Do not ignore them.
Likewise, reflect on your attitude towards those patients in the admission ward with deep vein thrombosis and ulcers from injecting drug misuse, or alcoholic hepatitis and cirrhosis. Unless you subscribe to the 'they get what they deserve' theory, maybe they are rather the modern equivalent of the many 'lepers' whom Jesus met, and touched. [8]
Peter Campion is emeritus professor of primary care at Hull York medical school